513
Views & Citations10
Likes & Shares
Material and methods: Class I cavities were prepared on 100 extracted molar teeth and were divided into two groups for microleakage (Group I) and fracture strength analysis (Group II) respectively. Each group was divided into 5 subgroups (IA IB IC ID IE and IIA IIB IIC IID IIE): Group IA, IIA restored with 2mm thick enamel slab+ composite; Group IB, IIB 1mm thick enamel slab+ composite; Group IC, IIC MTA+ RMGIC+ composite; GROUP ID, IID intact tooth; Group IE, IIE unrestored tooth. Samples of Group I was subjected to microleakage study by the dye penetration method and those of Group II were subjected to fracture strength analysis under the Universal Instron testing machine.
Results: The intact teeth and the group with 2mm thick enamel slab showed lowest microleakage with no statistically significant difference (p value< 0.005) between the two. MTA showed statistically significantly higher microleakage than these groups (p-value< 0.005). Significantly high fracture strength was observed in the intact tooth group followed by the group having 2mm thick enamel slab. However, MTA showed significantly lower fracture strength than groups with 2mm and 1mm thick enamel slab.
Conclusion: 2mm thick enamel slab is a novel pulp capping agent and can be considered as a potential alternative to conventional pulp capping agents.
Keywords: Pulp Capping, Substrate, Mineral Trioxide Aggregate, Enamel Slab
Mineral Trioxide Aggregate (MTA) has become popular as a pulp capping agent in recent years due to its antibacterial and biocompatibility properties, less solubility as it sets in the presence of moisture, osteo-induction and osteo-conduction and its ability to aid in the release of bioactive dentin matrix proteins [3]. The major disadvantage of MTA is its prolonged setting time. This requires that pulp capping with MTA either be done in a two-step procedure, placing a temporary restoration to allow the MTA to set before placing the permanent restoration, or using a quick-setting liner to protect the MTA during permanent restoration placement.
Using a natural substrate (enamel) as a pulp capping agent could be a possibility due to its better adhesion to restorative materials. In (1991) Santos and Bianchii [4] used the technique of bonding sterile tooth dental fragments to teeth with large coronal destruction. The term “Biological Restoration” was used to describe an alternative technique that uses adhesive capabilities of materials in combination with strategic placement of parts of extracted human permanent teeth to achieve better aesthetics and more conservation of sound dental tissues. The research in the field of biological restorations is still lacking. This study aims to evaluate enamel, a natural substrate as an alternative material for pulp capping and compare it with MTA by evaluating fracture strength and microleakage at the tooth-restoration interface in Class I cavities.
MATERIALS AND METHOD
This study was done in the Department of Conservative Dentistry and Endodontics, Sri Guru Ram Das Institute of Dental Sciences and Research, Sri Amritsar. Ethical clearance for which was obtained from the institutional ethical committee. Sample size was calculated by using formula i.e n=2*Z1-α/22 X SD2/d2 suggested by Charan and Biswas (2013). 140 extracted molar teeth were selected based on the following inclusion and exclusion criteria. Non-carious permanent mandibular molar teeth were included, whereas teeth with developmental defects, visible cracks, fractures, previously treated root canals, or any malformations were excluded from the study.
Procedure
Out of 140 selected teeth, 40 teeth were used for preparation of enamel slabs and on the other 100 teeth a Class I cavity was prepared using a No. 245 carbide bur, with a high-speed air rotor handpiece. The preparation extended 3-mm buccolingually and 4 mm mesiodistally with 4-mm pulpal depth. The samples were randomly divided into two groups: GROUP I for Microleakage study and GROUP II for Fracture strength analysis. In each of these groups 5 sub-groups were made depending upon the material used for pulp capping (n=10 samples in each sub-group) as classified in Table 1.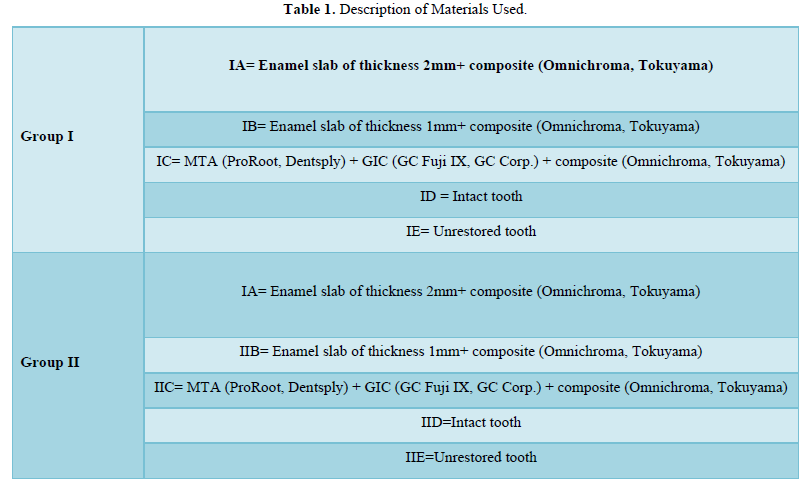
Sample Preparation
Preparation of enamel slab for SUB-GROUPs IA, IB, IIA, IIB - From 40 freshly extracted teeth 2 types of enamel slabs (n=10 each) one with dimensions 3mm buccolingually, 4mm mesiodistally and thickness of 1mm and the other with similar dimensions mesiodistally and buccolingually but greater thickness i.e., 2mm were obtained from the buccal or lingual aspects of extracted molars using a double side diamond coated disc.
Procedure
GROUP IA, IIA: Enamel slab of thickness 2mm (to be used as a pulp capping agent) was placed on the floor of the cavity. One coat of self-etch bonding agent (Palfique bond, Tokuyama) was applied and air dried for 5s followed by curing for 10s. The cavity was then restored with composite (Omni chroma, Tokuyama Dental) added in increments and each cured for 20s as per the manufacturer’s instructions.
GROUP IB, IIB: Enamel slab of thickness 1mm (to be used as a pulp capping agent) was placed on the floor of the cavity. One coat of self-etch bonding agent (Palfique bond, Tokuyama) was applied and air dried for 5s followed by curing for 10s. The cavity was then restored with composite (Omni chroma, Tokuyama Dental) added in increments and each cured for 20s.
GROUP IC, IIC: MTA (Pro Root, Dentsply) powder was mixed with distilled water on a glass slab according to manufacturer’s instructions and it was placed in the cavity using an amalgam carrier to a thickness of 1mm. After 45mins, GIC (GC Fuji IX, GC Corp.) was mixed according to manufacturer’s instructions, placed over MTA as a base. The rest of the cavity was restored with Omni chroma (Tokuyama Dental).
GROUP ID, IID Intact tooth: intact molar with no cavity preparation.
GROUP IE, IIE Unrestored tooth: class I cavity preparation was done on a molar tooth but no restorative material was placed in the cavity.
Thermocycling was done by alternating the samples in hot (fifty-five degree Celsius) and cold (five degrees Celsius) water baths with a dwell time of thirty seconds in each water bath and transfer time of 10 seconds between hot and Coldwater bath. Whole procedure was repeated for five hundred times i.e., total 500 cycles 5]. After thermocycling, the apices of the teeth were sealed with sticky wax to prevent dye to penetrate from the open apical areas of the prepared specimens.
Microleakage Testing
50 restored samples of subgroup IA IB IC ID IE (n=10 each) were subjected to the microleakage analysis by the dye penetration method. The specimens were dried and coated with nail varnish except for 0.5-1mm window around restoration margins and allowed to dry. Then the samples were immersed in 1% methylene blue dye for 24hrs and washed under running water for 30mins to rinse off the excess dye. Sectioning of the samples was done in the mesio-distal direction. The samples were observed under the stereomicroscope (MOTIC SMZ-143 SERIES) 40X and the extent of dye penetration was evaluated according to scoring criteria by Mazumdar [6].
- 0 no dye infiltration
- 1 dye penetration up to the first third of prepared cavity wall
- 2 dye penetration up to the second third of the prepared cavity wall
- 3 dye penetration onto the entire prepared cavity wall
- 4 dye penetration onto the entire prepared cavity wall and pulpal wall
Fracture Strength Analysis
50 restored samples of subgroup IIA IIB IIC IID IIE (n=10 each) were stored in deionized water for 24 h and then embedded in acrylic molds till the CEJ and subjected to fracture strength testing under the Universal Instron testing machine at crosshead speed of 1mm/min. Maximum force required to fracture was recorded.
All results of microleakage and fracture strength evaluation were put to statistical analysis using Post-hoc Bonferroni Test.
RESULTS
Microleakage Analysis
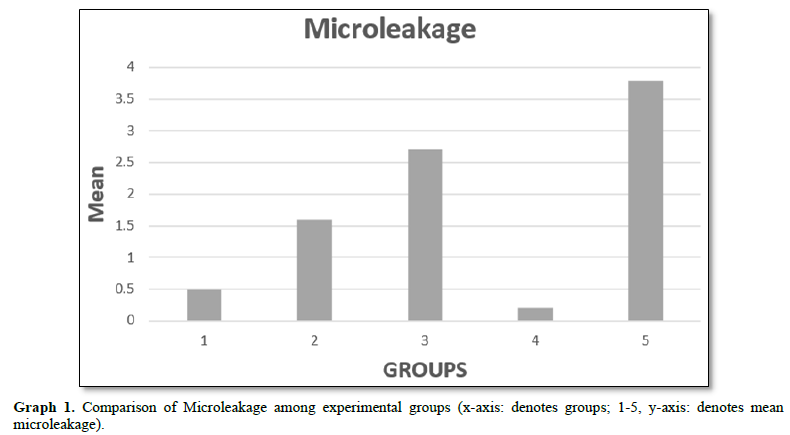
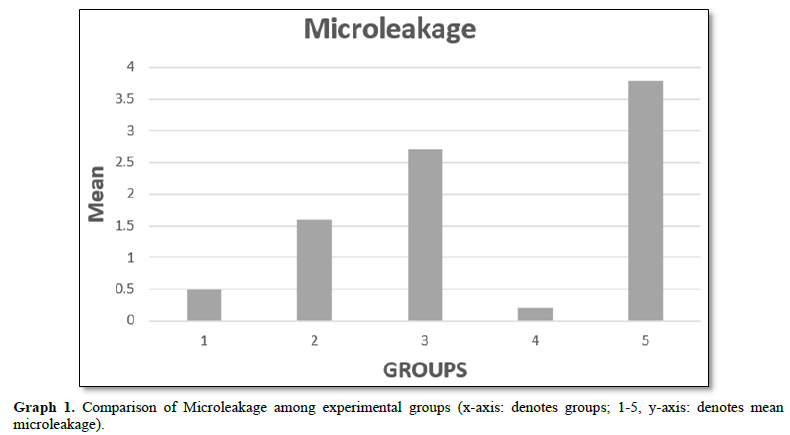
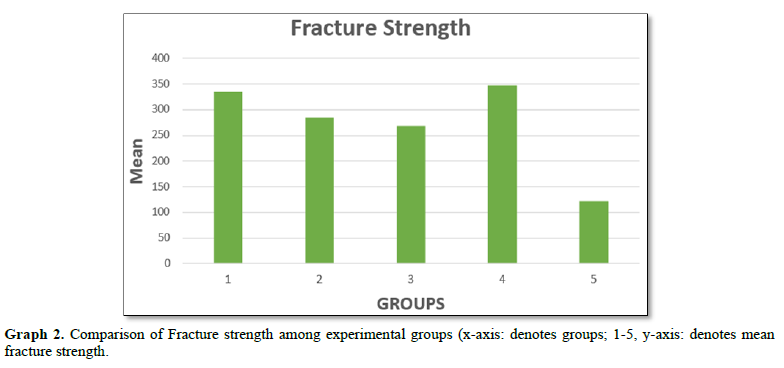
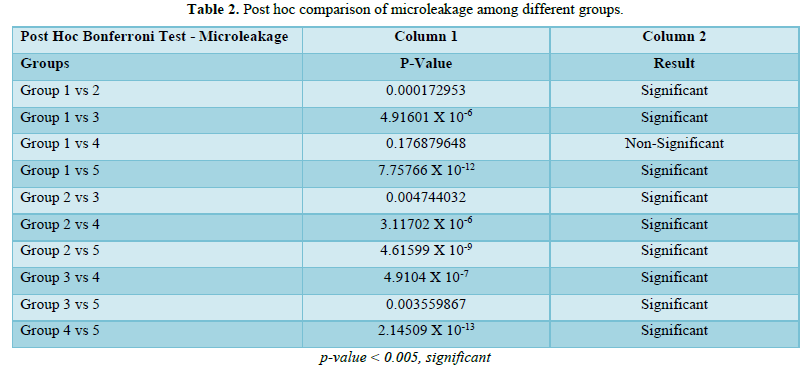
The lowest microleakage was observed in Group ID which was the intact tooth followed by Group IA (enamel slab of thickness 2mm). However, on statistical evaluation no statistically significant difference (p value< 0.005) was observed between these two groups. Group IB (enamel slab of thickness 1mm) had significantly higher microleakage (p value< 0.005) than Group IA and ID (Graph 1, Table 2).
Group IC (MTA with GIC) showed significantly higher microleakage (p value< 0.005) than Group ID (intact tooth), IA (enamel slab of 2mm thickness), IB (enamel slab of 1mm thickness). Highest microleakage was observed with the Group IE (unrestored tooth) which was significantly higher (p value< 0.005) than all other groups (Graph 1, Table 2).
Fracture Strength Analysis
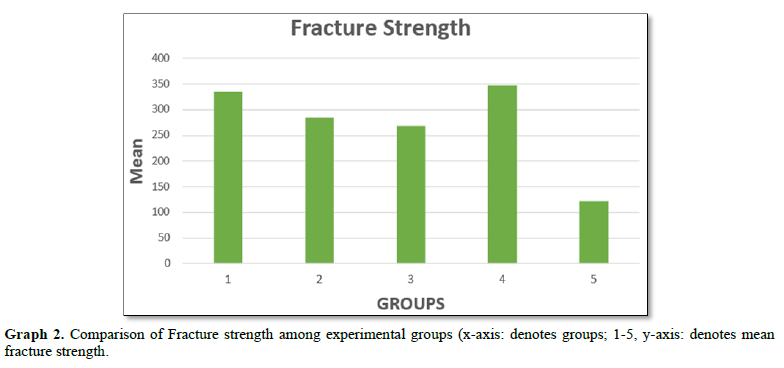
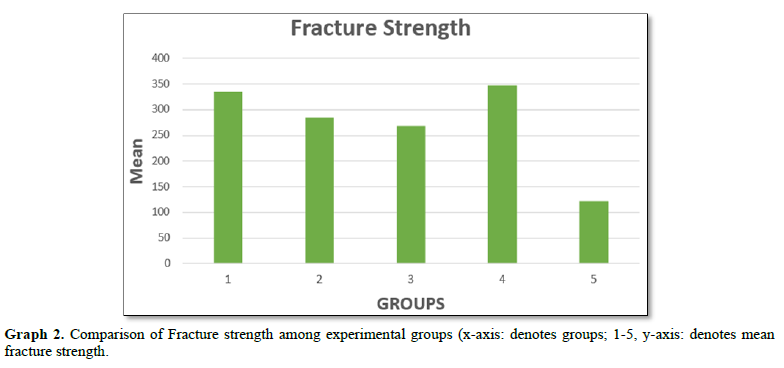
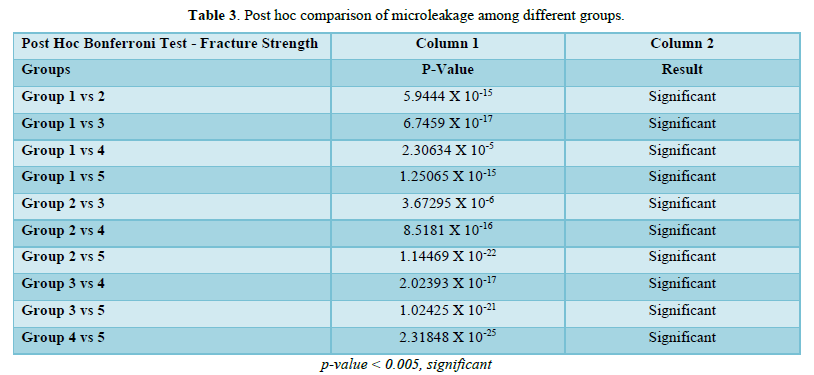
Highest Fracture strength was observed with Group IID (intact tooth) with a mean value of 347.2 MPa. Group IIA (enamel slab of 2mm thickness) showed lesser fracture strength than Group IID and there was a significant difference (p value< 0.005) between the two groups. Group IIB (enamel slab of 1mm thickness) showed lesser fracture strength than both Groups IID (intact tooth) and Group IIA (enamel slab of 2mm thickness) with a statistically significant difference (p value< 0.005) with both the groups. Group IIC showed mean fracture strength value of 268.5 which was lesser than Groups IIA, IID and IIB with a statistically significant difference between them (p value< 0.005). Lowest fracture strength was observed with Group IIE (unrestored tooth) which was significantly (p value <0.005) lower than all the groups (Graph 2, Table 3).
DISCUSSION
In this study microleakage and fracture strength of MTA was compared with natural tooth substrate (enamel slab) when used as pulp capping agents in deep cavities.
We chose self-etch Palfique Bond for this study as studies support the use of Universal bonding agents to bond GIC to composite. Gupta and Mahajan [7] in their study concluded that the application of self-etch bonding agent between GIC and composite resin increases the shear bond strength as compared to total etch type systems.
Omnichroma was used as a final restorative material for this study as it consists of spherical silica filers with uniform particle size of 260nm formed by SOL-GEL technique hence it shows better compressive strength and surface hardness. Thereby providing an adequate balance between esthetics and strength.
MTA, a highly biocompatible material which sets in the presence of moisture and forms a sound dentinal bridge is preferred for pulp capping [3]. However, the biggest drawback with MTA is its prolonged setting time of 2h and 45min [8,9] in their study compared the bond strength of composite with MTA at different time intervals and found that MTA has highest bond strength with composite after 24h with the total etch system and the lowest value after immediate application of MTA. In a study by Napte and Raghavendra S [10] it was seen that bond strength of MTA with GIC was comparable at 45 minutes and 72 h time interval that is why GIC was used as a base over MTA after 45 minutes in this study.
Enamel slab was chosen as an alternate to conventional materials as a pulp capping agent as it is a biological natural material thereby showing excellent biocompatibility, According to Beznos C [11] with enamel margins all materials and techniques demonstrated very good seal and less microleakage in contrast to cementum/dentin margins.
Microleakage results of our study showed that enamel slab of thickness 2mm exhibits less leakage as compared to MTA [12]. The mineralized structure of enamel presents distinct ultra-morphology and composition. Regardless of depth or where it is located enamel has crystal homogenous structure composed of hydroxyapatite (96% by wt and 86% by volume inorganic, 3%by wt/ 12% vol water, 1% wt/ 2% vol organic matrix). Higher mineral content of enamel allows more etching and hence better penetration of resin tags. Therefore, better bonding to restorative material. On the other hand, Cervino [13] analyzed the MTA- Adhesive interface under the scanning electron microscope and reported the presence of micro-gaps exhibiting unsatisfactory bonding at the MTA - Composite interface which promotes microleakage. Islam [14] stated that MTA has as a long setting time so it cannot be restored immediately.
Enamel slab of thickness 2mm exhibits less leakage as compared to enamel slab of thickness 1mm. Lesser the enamel more will be the composite resin hence more leakage. This was supported by Abrol [15] in their study found that all restored teeth exhibited certain amount of microleakage as compared to an intact tooth. The maximum microleakage was observed with the unrestored tooth.
Fracture Strength Analysis
In this study fracture strength of MTA was compared with natural tooth substrate (enamel slab) when used as pulp capping agents in deep cavities and it was found that the fracture strength of MTA was significantly lower than enamel slab. Balal [16] stated that the ProRoot MTA has higher molecular weight particles because of which it has lesser interfacial bonding with dentin and lesser tubular biomineralization which may be the reason for its reduced fracture strength. Calcium hydroxide formed as a by-product of the setting reaction of MTA may also be responsible for its reduced fracture strength.
The fracture strength of 2mm thick enamel slab was more than that of 1mm thick enamel slab because decrease in the thickness of enamel and increase in the resin composite values reduced the fracture strength of the tooth.
The fracture strength of 2mm thick enamel was significantly less than that of intact tooth. This is in accordance with the results of the study published by Forster [17] which showed that the fracture strength of the intact tooth is higher than restored tooth. In this study this may be due to operative procedures like the loss of tooth structure during cavity preparation, smear layer formation and presence of composite restorative material.
CONCLUSION
2 mm enamel slab used as pulp capping agent showed significantly lower microleakage as compared to 1mm enamel slab and MTA.
2 mm enamel slab used as pulp capping agent showed significantly higher fracture strength as compared to 1mm enamel slab and MTA.
Thus, it can be concluded from the present study that 2mm enamel slab is a novel natural pulp capping agent and can be considered as a potential alternative to conventional synthetic pulp capping agents. Further long-term In-Vivo studies should be done to evaluate its clinical application.
- Hilton TJ (2009) Keys to clinical success with pulp capping: A review of the literature. Oper Dent 34: 615-625.
- Nowicka A, Wilk G, Lipski M, Kołecki J, Buczkowska-Radlińska J (2015) Tomographic evaluation of reparative dentin formation after direct pulp capping with Ca(OH)2, MTA, Biodentine, and dentin bonding system in human teeth. J Endod 41(8): 1234-1240.
- Malhotra N, Agarwal A, Mala K (2013) Mineral trioxide aggregate: A review of physical properties. Compend Contin Educ Dent 34(2): e25-e32.
- Santos JFF, Bianchi J (1992) Biologic esthetic restorations. J Esthet Dent 4: 1-3.
- Wahab FK, Shaini FJ, Morgano SM (2003) The effect of thermocycling on microleakage of several commercially available composite Class V restorations in vitro. J Prosthet Dent 90(2): 168-174.
- Mazumdar P, Das A, Das UK (2019) Comparative evaluation of microleakage of three different direct restorative materials (silver amalgam, glass ionomer cement, Cention N), in class II restorations using stereomicroscope: an in vitro Indian J Dent Res 30(2): 277.
- Gupta R, Mahajan S (2015) Shear bond strength evaluation of resin composite bonded to GIC using different adhesives. J Clin Diagn Res 9(1): ZC27-ZC29.
- Banava S, Janfeshan Z, Saghiri AM (2013) In-vitro comparison of primary setting time and surface porosity of two types of Mineral Trioxide Aggregate (MTA). J Iran Dent Assoc 25(1): 1-5.
- Sulwińska M, Szczesio A, Bołtacz-Rzepkowska E (2017) Bond strength of a resin composite to MTA at various time intervals and with different adhesive strategies. Dent Med 54(2): 155-160.
- Napte BD, Raghavendra SS (2015) Evaluation of shear bond strength of conventional glass ionomer cements bonded to mineral trioxide aggregate: An in vitro J Dent Allied Sci 4(2): 73.
- Beznos C (2001) Microleakage at the cervical margin of composite Class II cavities with different restorative techniques. Oper Dent 26(1): 60-69.
- Kaur R, Goyal S, Sahiwal H, Grover JS, Bhullar KK, et al. (2023) Newer Possibilities for Proximal Box Elevation-Tooth Substrate and Comparison with Conventional Materials: An Ex-vivo J Pharm Res Int 35(10): 34-39.
- Cervino G, Fiorillo L, Spagnuolo G, Bramanti E, Laino L, et al. (2017) Interface between MTA and dental bonding agents: Scanning electron microscope evaluation. J Int Soc Prev Community Dent 7(1): 64.
- Islam I, Chng HK, Yap AUJ (2006) X‐ray diffraction analysis of mineral trioxide aggregate and Portland cement. Int Endod J 39(3): 220-225.
- Abrol A, Aggarwal N, Gupta P, Kunjam M, Abrol N (2019) Comparative evaluation of microleakage around class ii cavities restored with Zirconomer, Tetric N Ceram, Cention-N and glass ionomer cement-an in vitro Int J Curr Res 1(02): 1641-1644.
- Ballal NV, Gandhi P, Shenoy PA, Dummer PM (2020) Evaluation of various irrigation activation systems to eliminate bacteria from the root canal system: A randomized controlled single blinded trial. J Dent 99: 103412.
- Forster A, Braunitzer G, Tóth M, Szabó BP, Fráter M (2019) In vitro fracture resistance of adhesively restored molar teeth with different MOD cavity dimensions. J Prosthodont 28(1): e325-e331.